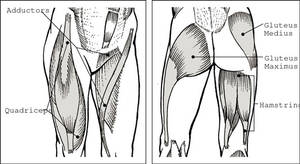
The calf muscle is found at the back of the lower leg and is consisted of three muscles: the plantaris, the gastrocnemius and the soleus. These 3 muscles are referred to as ‘the tricep muscles surae’, and they attach to the Achilles tendon. Strained calf muscle laso known as pulled calf muscle. We will talk about this issue in this short article.
They are responsible for extending the foot (plantar flexion) and flexing the leg at the knee joint.
The Achilles tendon connects to the heel bone (the calcaneus). The soleus sits deep to the gastrocnemius, with the plantaris muscle and part of its tendon located between these two muscles.
A calf strain occurs as an outcome of these muscles being torn or pulled. When a muscle is extended, small micro tears happen in the muscle fibers. The severity of these tears depends on the depth and suddenness of the stretch. There are three different degrees of calf strain: grade 1 is a moderate strain, grade 2 moderate to severe pain and a grade 3 strain is a complete rupture.
Causes
- A calf strain happens when the calf muscles are over stretched. This can be caused by a sudden, abrupt motion or as an outcome of over use.
- Insufficient heat up or cool down is a typical cause of calf strain.
- An unexpected modification of instructions, explosive motion or increase in speed can result in the calf muscles becoming torn or strained.
- Climbing up or adding hills.
- Over pronation.
- Wearing improper footwear.
Symptoms
- Problem weight bearing.
- A burning/stabbing sensation.
- A sensation of being hit on the back of the lower leg.
- Pain on withstood plantar flexion (pointed toe) or when basing on pointed toes.
- A sudden sharp pain in the lower leg.
- Bruising to the lower leg, as an outcome of internal bleeding.
- Inflammation of the lower leg.
- Tightness.
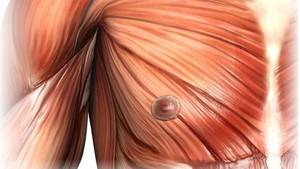
- A lump can be felt.
- Pain/ache in the calf, generally mid calf.
In a Grade 1 degree strain
- Small swelling and bruising.
- The muscles can feel tight and pains when extended.
- Pain/discomfort can be felt after the activity, and can last from between 2-5 days
In a Grade 2 degree strain
- The pain is instant.
- The muscle can be tender to touch.
- There is inflammation.
- A few days after the injury, bruising will appear below where the partial tear has actually taken place.
- The muscle feels tight and painful on resisted plantar flexion (pointing the toe).
In a Grade 3 degree strain (a complete rupture)
- Pain is felt instantly, and can feel like a burning or stabbing sensation.
- The muscle is tender to touch.
- Inflammation happens.
- A lump of muscle tissue can be felt where the tear has actually occurred.
- A few days after the injury, bruising will appear below where the rupture has happened.
- Pain is felt when walking or weight bearing.
- Unable to contract the muscle, as the muscle has burst completely.
How Is Strained Calf Muscle Treated?
- It is important not to neglect a calf strain, as this might cause further damage and cause a grade 3 strain. The earlier the treatment, the better the result. In a grade 1 strain recovery is roughly 2 weeks. In a grade 2 strain, recovery can use up to 5-8 weeks, and for grade 3 stress can take up to 3-4 months.
- Rest: to prevent more damage.
- In the sub acute (3 days to 3 weeks) and the chronic stage (3 weeks to 2 years) it is important that training must be adjusted to prevent leaping or any exercises that put excessive strain on the gastrocnemius or soleus.
A physiotherapist or sportsmassage therapist or sports therapist can advise when exercise needs to be resumed and what workout would be suitable.
- Ice treatment: Ice, can be requested 10-15 minutes, every 2-3 hours in the acute and sub- acute stage (frequency can be lowered inning accordance with recovery, and can be continued for as long as deemed necessary). Ice bands are an efficient method of applying ice therapy. In the sub-acute stage (3days — 3 weeks) heat therapy can be applied.
- Compression: to decrease swelling and limit movement.
- Strapping offers support. In a total rupture the doctor might prescribe a cast to provide stability.
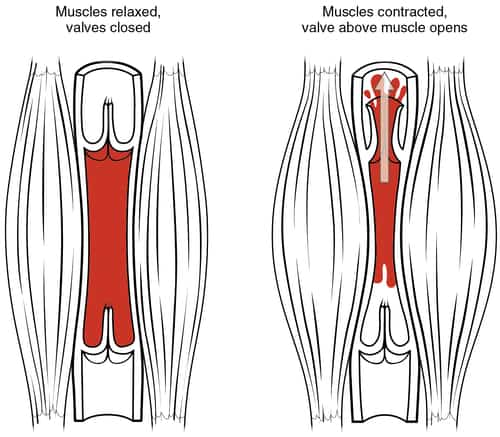
- Elevation: Gravity will help lymphatic drainage and help venous return.
- NSAIDS (anti-inflammatories) and paracetamol can be required to aid pain relief. Medical recommendations needs to be looked for, in case of possible side effects.
- Orthotics can prevent overprontation. It is for that reason, worth consulting a podiatrist, who can carry out gait analysis and recommend on suitable foot wear.
Kinesiology taping aids recovery by assisting with lymphatic drain, and the repair of broken tissues.
A doctor or physiotherapist may recommend an MRI scan to examine the extent of rupture. In severe cases surgery might be performed.
A physio therapist might recommend ultrasound treatment, acoustic waves; which speeds up the repair process, by breaking down tissues and stretching them. It can also help relieve pain.
Massage can assist recovery, and enhance joint movement and variety of movement. It ought to not be administered during the acute stage. If there is any underlying medical condition, such as a heart disease, it is very important to seek medical suggestions before receiving massage.
A physio therapist or sports massage therapist can suggest strengthening, versatility and proprioceptive exercises in the sub-acute and the chronic stage of recovery. Exercises need to concentrate on extending and strengthening, focusing on the gastrocnemius and soleus muscles; for example calf and toe raises. The intensity of the exercises must be increased slowly and in a regulated method. Resistance bands benefit mild extending.
For injury avoidance, it is essential that a warm up and cool off types part of a workout programme (10-20 minutes, depending on the duration of the program).