A Pap smear, also known as a Pap test, is a routine screening procedure primarily used to detect cervical cancer and precancerous changes in the cervix. During the test, a healthcare provider collects cells from the cervix using a small brush or spatula. These cells are then analyzed under a microscope for abnormalities.
Prevalence of STDs Among Women Undergoing Pap Smear Tests (2023, USA)
| STD | Prevalence (%) |
|---|---|
| Chlamydia | 12% |
| HPV (High-risk strains) | 22% |
| Gonorrhea | 4% |
| Trichomoniasis | 3% |
| Herpes (HSV-2) | 9% |
| HIV | 0.5% |
This chart shows the prevalence of various sexually transmitted diseases (STDs) among women in the United States who underwent Pap smear tests in 2023. HPV and Chlamydia were the most common, while HIV had the lowest detected prevalence. Bar widths are scaled for clear visual comparison.
The main purpose of a Pap smear is to catch early signs of cervical dysplasia and human papillomavirus (HPV)-related changes, helping prevent cervical cancer. It’s recommended every 3 years for women aged 21–65, or every 5 years when combined with HPV testing.
So, Can a Pap Smear Detect STDs?
Short answer: not directly.
A Pap smear is not designed to diagnose sexually transmitted diseases (STDs). However, it can sometimes hint at the presence of infections through the observation of inflammation or cellular changes, prompting further testing. Some labs may simultaneously test for HPV, a sexually transmitted virus, during the Pap smear, but this requires explicit instruction from the healthcare provider.
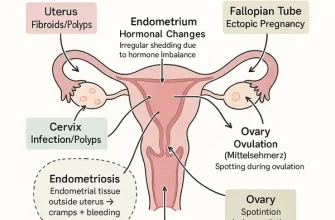
STDs That May Be Indirectly Detected
While not a direct diagnostic tool, a Pap smear might reveal signs that warrant STD testing, such as:
| STD | Can It Be Found in Pap? | Requires Separate Test? | Common Test Method |
|---|---|---|---|
| HPV | Yes (if co-tested) | Often co-tested | DNA test / PCR |
| Chlamydia | No | Yes | NAAT (nucleic acid test) |
| Gonorrhea | No | Yes | NAAT |
| Trichomoniasis | Rarely | Yes | Wet mount / NAAT |
| Herpes (HSV) | No | Yes | Blood test / PCR |
| Syphilis | No | Yes | Blood test |
HPV Types Most Frequently Detected During Pap Smear Screening
The chart highlights the most frequently detected high-risk HPV types during Pap smear screenings. HPV-16 is the most prevalent, followed by HPV-18 and a mix of other oncogenic strains. The data emphasizes the importance of targeted HPV vaccination and regular screening.
The Role of HPV in Pap Smear Results
Human papillomavirus (HPV) is the only STD that a Pap smear can routinely co-detect if requested. High-risk strains of HPV are linked to cervical cancer. According to the CDC, over 42 million Americans are infected with HPV, and nearly everyone will contract it at some point in their lives.
When HPV testing is included:
- Accuracy: 9.5/10
- Average cost: $75–$150 (depending on lab)
Diagnostic Tools for Accurate STD Detection
Here’s what’s used when precise STD testing is needed:
NAAT (Nucleic Acid Amplification Test)
- Used For: Chlamydia, Gonorrhea, Trichomoniasis
- Accuracy: 9.8/10
- How It Works: Detects genetic material of pathogens in urine or swabs
- Average Cost: $100–$250
PCR Testing
- Used For: HPV, Herpes
- Accuracy: 9.7/10
- How It Works: Amplifies DNA segments for detection
- Average Cost: $130–$200
Blood Tests
- Used For: Syphilis, Herpes (antibody detection)
- Accuracy: 9.0/10
- How It Works: Detects antibodies or antigens in the bloodstream
- Average Cost: $50–$120
Real Cases From U.S. Clinics
- A 28-year-old woman from Atlanta had a routine Pap smear that showed atypical squamous cells. Co-testing revealed high-risk HPV, and subsequent testing confirmed early-stage cervical dysplasia.
- A 33-year-old woman in Phoenix reported recurrent vaginal discharge. Though her Pap smear was normal, follow-up testing confirmed trichomoniasis.
Expert Tips: How to Get the Most From Your Gynecological Visit
- Ask for HPV testing along with your Pap smear if you’re over 30.
- Request comprehensive STD screening if you’re sexually active with new or multiple partners.
- Communicate any unusual symptoms like discharge, itching, or discomfort.
Editorial Advice
Reyus Mammadli, healthcare advisor, recommends: “Don’t assume a normal Pap smear means you’re free of STDs. Be proactive and ask your provider for full STD testing, especially if you’ve had new partners or symptoms.”
It’s a smart move to combine your regular gynecological exam with a full panel of STD tests. This ensures comprehensive reproductive health screening. Clinics now offer combo packages that include Pap smears and NAATs, which can be both efficient and cost-effective.
STDs That Can Be Co-Tested with Pap Smear in Routine Exams
This chart displays common STD tests that can be co-administered with a Pap smear during routine gynecological exams. HPV DNA testing is universal, while others like Chlamydia, Gonorrhea, and HIV are selectively included based on patient risk factors and provider guidelines.
References
MedlinePlus (U.S. National Library of Medicine). “Nucleic Acid Amplification Tests (NAATs).”
https://medlineplus.gov/lab-tests/nucleic-acid-amplification-tests-naats/
Centers for Disease Control and Prevention (CDC). “STD Facts – Human Papillomavirus (HPV).”
https://www.cdc.gov/std/hpv/stdfact-hpv.htm
American College of Obstetricians and Gynecologists (ACOG). “Cervical Cancer Screening.”
https://www.acog.org/womens-health/faqs/cervical-cancer-screening
Mayo Clinic. “Pap smear: Purpose, Procedure and Results.”
https://www.mayoclinic.org/tests-procedures/pap-smear/about/pac-20394841
U.S. Preventive Services Task Force. “Cervical Cancer: Screening.”
https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/cervical-cancer-screening
Cleveland Clinic. “STD Testing.”
https://my.clevelandclinic.org/health/diagnostics/15170-std-testing