Fibromyalgia is a complex condition that leaves sufferers with persistent, widespread pain. Understanding whether this pain is acute or chronic is crucial for proper management and treatment.
Age Group Distribution of Fibromyalgia Cases
| Age Group | Prevalence (%) |
|---|---|
| 18 – 29 | 10% |
| 30 – 39 | 25% |
| 40 – 49 | 35% |
| 50 – 59 | 50% |
| 60+ | 60% |
This chart illustrates the estimated prevalence of fibromyalgia across different age groups. Symptoms often become more noticeable with age, but younger individuals can also be affected.
What Is Fibromyalgia?
Fibromyalgia is a disorder characterized by:
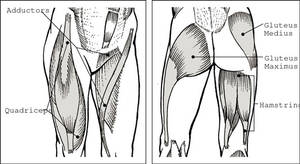
- Widespread pain: Persistent aches and tender points throughout the body.
- Fatigue: Even after long hours of sleep, patients often wake up feeling unrefreshed.
- Cognitive difficulties: Commonly referred to as “fibro fog,” affecting concentration and memory.
The condition remains poorly understood, with no single test to confirm its presence. Instead, diagnosis is based on clinical evaluation and the exclusion of other conditions.
What Is Pain? Acute vs. Chronic
Pain is the body’s way of signaling that something is wrong. It can be classified into two categories:
- Acute Pain:
- Onset: Sudden, often linked to an injury or a specific event.
- Duration: Short-term, usually subsiding within a couple of weeks.
- Function: Serves as a protective mechanism to prevent further injury.
- Chronic Pain:
- Onset: Develops over time and persists beyond the expected healing period.
- Duration: Lasts for months or even years.
- Impact: Can significantly affect daily activities, mood, and quality of life.
In fibromyalgia, while patients might experience sudden flare-ups resembling acute pain, the underlying condition is marked by chronic pain that lingers and affects every aspect of life.
How the Brain Processes Fibromyalgia Pain
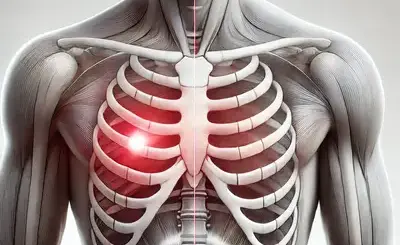
Our nervous system is equipped with various nerve endings that transmit signals to the brain. In fibromyalgia:
- Altered Pain Processing: The brain’s pain-processing centers may misinterpret non-painful signals as painful.
- Hypersensitivity: Even normal stimuli can trigger significant discomfort.
- Blood Flow Changes: Research shows that reduced blood flow to certain brain areas may impair pain regulation, contributing to persistent, widespread pain.
These factors combine to make fibromyalgia a uniquely challenging condition to manage.
Acute vs. Chronic Pain in Fibromyalgia
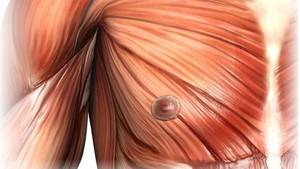
While fibromyalgia is predominantly associated with chronic pain, it’s important to recognize that:
- Acute Flare-Ups: Patients may experience bursts of severe pain, especially after physical or emotional stress.
- Chronic Baseline: Despite these flare-ups, the overall pain remains a long-term, ongoing issue.
Understanding this distinction helps in designing a treatment strategy that addresses both immediate discomfort and long-term management.
Severity of Fibromyalgia Symptoms
| Symptom | Intensity (%) |
|---|---|
| Chronic Muscle Pain | 80% |
| Fatigue | 70% |
| Sleep Disturbances | 65% |
| Morning Stiffness | 60% |
| Fibro Fog | 55% |
| Headaches | 50% |
This chart illustrates the symptoms that people with fibromyalgia most commonly report as severe. It can help prioritize treatment and self-care strategies to target the most debilitating aspects first.
Treatment and Management Strategies
Effectively managing fibromyalgia pain requires a multifaceted approach:
- Medications:
- Analgesics: Over-the-counter pain relievers or prescribed medications.
- Antidepressants and Anticonvulsants: Often used to modulate pain signals and improve sleep quality.
- Physical Therapy:
- Exercise: Low-impact activities like walking, swimming, or yoga can help reduce pain and improve mobility.
- Stretching: Regular gentle stretching can ease muscle tension.
- Psychological Support:
- Cognitive Behavioral Therapy (CBT): Helps in managing the mental stress and anxiety associated with chronic pain.
- Mind-Body Techniques: Practices like meditation and deep breathing support overall well-being.
- Lifestyle Adjustments:
- Sleep Hygiene: Improving sleep patterns can reduce the intensity of pain.
- Diet and Hydration: A balanced diet and adequate water intake may lessen inflammation.
- Alternative Therapies:
- Acupuncture and Massage: These therapies can complement conventional treatments by reducing muscle tension and improving circulation.
Treatment Methods and Their Effectiveness
| Method | Effectiveness (%) |
|---|---|
| Medications | 80% |
| Exercise Therapy | 75% |
| Cognitive Behavioral Therapy | 70% |
| Massage Therapy | 65% |
| Diet and Nutrition | 60% |
| Stress Management Techniques | 50% |
This chart compares various fibromyalgia treatment methods based on reported effectiveness. While medications may be most effective for some, a holistic approach often involves combining exercise, therapy, diet changes, and stress management for better overall results.
Living with Fibromyalgia: Daily Tips
- Pace Yourself: Avoid overexertion. Listen to your body and rest when needed.
- Stay Active: Regular, moderate exercise is key to reducing pain and improving mood.
- Manage Stress: Techniques such as mindfulness, yoga, or counseling can be beneficial.
- Support Network: Connect with friends, family, or support groups for shared experiences and encouragement.
Editorial Advice
Fibromyalgia is a complex condition that affects both physical and emotional well-being. A comprehensive treatment plan that goes beyond just medication is key to managing this chronic condition.
- Statistics: Research shows that fibromyalgia affects approximately 2–4% of the population, with women accounting for 80–90% of cases. Additionally, multidisciplinary approaches that combine medication, physical therapy, and stress management have been shown to reduce pain intensity by up to 30% in many patients.
If you or someone you know is struggling with fibromyalgia, consult a healthcare professional to develop a personalized, holistic management strategy.
FAQ
1. What factors can trigger flare-ups in fibromyalgia symptoms?
Fibromyalgia flare-ups can be triggered by emotional stress, physical overexertion, sudden weather changes, or insufficient rest. These factors may increase the sensitivity of your nervous system, leading to more intense pain episodes.
2. Is there a genetic predisposition to fibromyalgia?
Some studies suggest a hereditary component, as fibromyalgia symptoms often occur among family members. However, no single gene has been identified as the definitive cause, indicating that genetics likely play a role alongside environmental factors.
3. How do hormonal changes influence fibromyalgia symptoms?
Hormonal imbalances—especially those related to stress hormones and thyroid function—can heighten pain sensitivity and exacerbate symptoms. Women, in particular, may experience more pronounced effects due to natural hormonal fluctuations.
4. Can diet affect fibromyalgia symptoms?
Yes, diet can have a significant impact. A balanced diet rich in omega-3 fatty acids, antioxidants, and anti-inflammatory foods may help reduce symptom severity. Some patients find that avoiding processed foods and sugar leads to an improvement in their overall condition.
5. How does sleep quality impact fibromyalgia patients?
Poor sleep quality or insufficient sleep can worsen pain, fatigue, and cognitive difficulties. Establishing a regular sleep schedule and creating a calming bedtime routine are crucial steps in managing fibromyalgia symptoms.
6. What modern diagnostic methods are used to identify fibromyalgia?
Diagnosis is typically based on a comprehensive clinical evaluation, including a detailed patient history and the exclusion of other conditions. Healthcare providers may also use specialized questionnaires and lab tests to assess the overall symptom profile.
7. How does fibromyalgia affect mental health?
Living with chronic pain can lead to increased levels of anxiety, depression, and social isolation. Many patients benefit from psychological support, such as cognitive behavioral therapy (CBT) and stress management techniques, to help cope with the mental health challenges associated with the condition.
8. What alternative therapies may benefit fibromyalgia patients?
In addition to traditional treatments, alternative therapies like acupuncture, massage, yoga, and meditation can help alleviate muscle tension, improve circulation, and reduce stress. These complementary methods are often used alongside medical treatment for a more holistic approach.
9. How does physical activity influence fibromyalgia symptoms?
Moderate physical activities—such as walking, swimming, or gentle stretching—can improve circulation and reduce muscle stiffness. It’s important to balance activity with rest, as overexertion may lead to symptom flare-ups.
10. What are the long-term prospects for individuals with fibromyalgia?
While fibromyalgia is a chronic condition, many patients experience significant improvement in their quality of life with proper treatment. A comprehensive approach that includes medication, lifestyle changes, and psychological support can help manage symptoms over the long term.
11. What steps can be taken to prevent symptom exacerbation in fibromyalgia?
Preventative measures include maintaining a regular sleep routine, managing stress through mindfulness or therapy, following a balanced diet, and engaging in regular, moderate exercise. These steps can help stabilize symptoms and reduce the frequency of flare-ups.
12. How do fibromyalgia symptoms differ between men and women?
Fibromyalgia is more commonly diagnosed in women, often due to hormonal influences, but men can also be affected. Men may experience less pronounced symptoms, which can sometimes lead to underdiagnosis. However, the impact on quality of life can be equally significant regardless of gender.