Guillain-Barre (gee-YAH-buh-RAY) syndrome is an uncommon disorder where your body’s body immune system attacks your nerves. Weakness and tingling in your extremities are typically the first symptoms.These experiences can rapidly spread, ultimately disabling your whole body. In its most severe type Guillain-Barre syndrome is a medical emergency situation. Many people with the condition need to be hospitalized to receive treatment.
The precise cause of Guillain-Barre syndrome is unidentified. But it is often preceded by a transmittable disease such as a respiratory infection or the stomach influenza. There’s no recognized treatment for Guillain-Barre syndrome, however a number of treatments can alleviate symptoms and lower the duration of the disease. The majority of people recuperate from Guillain-Barre syndrome, though some might experience remaining impacts from it, such as weak point, numbness or fatigue.
Symptoms
Guillain-Barre syndrome frequently begins with tingling and weak point starting in your feet and legs and infecting your upper body and arms. In about half of people with the disorder, symptoms start in the arms or face. As Guillain-Barre syndrome progresses, muscle weakness can progress into paralysis.
Signs and symptoms of Guillain-Barre syndrome may include:
- Prickling, pins and needles sensations in your fingers, toes, ankles or wrists
- Unstable walking or failure to walk or climb up stairs
- Rapid heart rate
- Problem breathing
- Weak point in your legs that spreads to your upper body
- Severe pain that might feel throbbing or cramplike and might be even worse during the night
- Problem with bladder control or bowel function
- Trouble with eye or facial movements, including speaking, chewing or swallowing
- Low or high blood pressure
People with Guillain-Barre syndrome typically experience their most considerable weak point within two to four weeks after symptoms start.
Types
Once believed to be a single disorder, Guillain-Barre syndrome is now known to happen in a number of kinds. The primary types are:
- Acute inflammatory demyelinating polyradiculoneuropathy (AIDP), the most typical kind in the United States. The most typical sign of AIDP is muscle weak point that begins in the lower part of your body and spreads up.
- Miller Fisher syndrome (MFS), in which paralysis begins in the eyes. MFS is likewise associated with unstable gait. MFS takes place in about 5 percent of people with Guillain-Barre syndrome in the United States however is more common in Asia.
- Acute motor axonal neuropathy (AMAN) and acute motor-sensory axonal neuropathy (AMSAN) are less typical in the United States. However AMAN and AMSAN are more frequent in China, Japan and Mexico.
When to see a doctor
Call your doctor if you have mild tingling in your toes or fingers that doesn’t seem to be spreading or becoming worse. Seek emergency situation medical help if you have any of these severe signs or symptoms:
- Tingling that begun in your feet or toes and is now moving up your body
- Tingling or weak point that’s spreading rapidly
- Trouble catching your breath or shortness of breath when lying flat
- Choking on saliva
Guillain-Barre syndrome is a severe condition that requires instant hospitalization since it can worsen quickly. The faster appropriate treatment is started, the better the possibility of a good result.
Causes of Guillain-Barre Syndrome
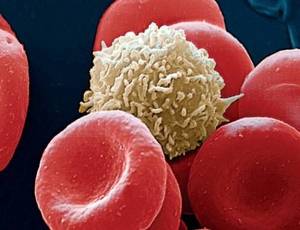
The specific cause of Guillain-Barre syndrome isn’t known. The disorder normally appears days or weeks after a breathing or gastrointestinal tract infection. Hardly ever, recent surgery or immunization can activate Guillain-Barre syndrome. Just recently, there have been a few cases reported following infection with the Zika virus. In Guillain-Barre syndrome, your immune system — which generally attacks only invading organisms– begins attacking the nerves. In AIDP, the most typical kind of Guillain-Barre syndrome in the United States, the nerves’ protective covering (myelin sheath) is harmed. The damage prevents nerves from transferring signals to your brain, causing weakness, numbness or paralysis.
Risk factors
Guillain-Barre syndrome can affect any age groups. But you’re at somewhat greater risk if you’re a man or a young adult.
Guillain-Barre syndrome may be triggered by:
- Epstein-Barr virus
- Hodgkin’s lymphoma.
- Hepatitis A, B, C and E.
- Surgery.
- Zika infection
- The majority of commonly, infection with campylobacter, a type of bacteria frequently discovered in undercooked poultry
- HIV, the infection that causes AIDS.
- Mycoplasma pneumonia.
- Cytomegalovirus
- Hardly ever, influenza vaccinations or childhood vaccinations.
- Influenza infection
Complications
Guillain-Barre syndrome impacts your nerves. Because nerves manage your movements and body functions, people with Guillain-Barre may experience:
- Breathing difficulties. The weak point or paralysis can infect the muscles that manage your breathing, a potentially deadly issue. As much as 30 percent of people with Guillain-Barre syndrome need temporary help from a maker to breathe when they’re hospitalized for treatment.
- Recurring numbness or other experiences. Most people with Guillain-Barre syndrome recuperate totally or have only small, residual weak point, numbness or tingling.
- Heart and high blood pressure problems. High blood pressure changes and irregular heart rhythms (cardiac arrhythmias) are common side effects of Guillain-Barre syndrome.
- Pain. Approximately half of people with Guillain-Barre syndrome experience severe nerve pain, which might be relieved with medication.
- Bowel and bladder function issues. Slow bowel function and urine retention may arise from Guillain-Barre syndrome.
- Embolism. People who are immobile due to Guillain-Barre syndrome are at risk of developing blood clots. Till you’re able to walk independently, taking blood slimmers and wearing support stockings might be recommended.
- Pressure sores. Being immobile likewise puts you at risk of establishing bedsores (pressure sores). Regular repositioning might assist prevent this issue.
- Relapse. Around 3 percent of people with Guillain-Barre syndrome experience a regression.
Severe, early symptoms of Guillain-Barre syndrome substantially increase the risk of severe long-lasting complications. Hardly ever, death may occur from complications such as respiratory distress syndrome and heart attack.
Diagnosis
Guillain-Barre syndrome can be hard to detect in its earliest stages. Its symptoms and signs are similar to those of other neurological conditions and might vary from individual to person.
Your doctor is most likely to start with a case history and thorough health examination.
Your doctor may then advise:.
- Spinal tap (lumbar puncture). A small amount of fluid is withdrawn from the spine canal in your lower back. The fluid is evaluated for a kind of change that commonly happens in people who have Guillain-Barre syndrome.
- Electromyography. Thin-needle electrodes are inserted into the muscles your doctor wishes to study. The electrodes procedure nerve activity in the muscles.
- Nerve conduction research studies. Electrodes are taped to the skin above your nerves. A small shock is passed through the nerve to measure the speed of nerve signals.
Treatment for Guillain-Barre Syndrome
There’s no cure for Guillain-Barre syndrome. But two types of treatments can speed recovery and decrease the severity of the disease:
- Plasma exchange (plasmapheresis). The liquid portion of part of your blood (plasma) is gotten rid of and separated from your blood cells. The blood cells are then return into your body, which makes more plasma to make up for what was eliminated. Plasmapheresis might work by ridding plasma of certain antibodies that add to the immune system’s attack on the peripheral nerves.
- Immunoglobulin therapy. Immunoglobulin consisting of healthy antibodies from blood donors is provided through a vein (intravenously). High doses of immunoglobulin can obstruct the destructive antibodies that might contribute to Guillain-Barre syndrome.
These treatments are equally effective. Blending them or administering one after the other disappears reliable than using either approach alone.
You also are likely to be given medication to:
- Eliminate pain, which can be severe.
- Prevent blood clots, which can develop while you’re immobile.
People with Guillain-Barre syndrome need physical assistance and therapy prior to and during recovery. Your care may include:
- Motion of your limbs by caretakers prior to recovery, to help keep your muscles flexible and strong.
- Physical therapy during recovery to assist you manage fatigue and restore strength and correct movement.
- Training with adaptive devices, such as a wheelchair or braces, to offer you mobility and self-care skills.
Recovery
Although some people can take months as well as years to recuperate, most people with. Guillain-Barre syndrome experience this basic timeline:
- After the first signs and symptoms, the condition tends to gradually intensify for about two weeks.
- Symptoms reach a plateau within four weeks.
- Recovery begins, normally lasting 6 to 12 months, though for some people it might take as long as three years.
Amongst adults recuperating from Guillain-Barre syndrome:
- About 80 percent can walk individually 6 months after medical diagnosis.
- About 60 percent totally recover motor strength one year after medical diagnosis.
- About 5 to 10 percent have really delayed and insufficient recovery.
- Children, who seldom develop Guillain-Barre syndrome, typically recuperate more completely than adults.