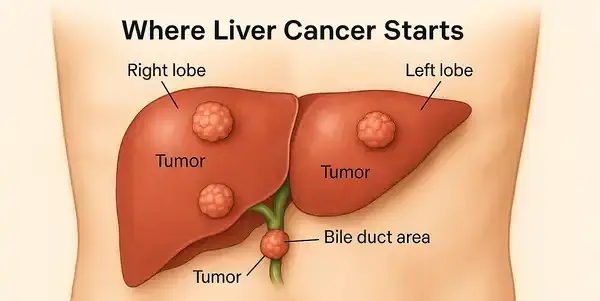
Liver cancer, also called hepatic cancer, originates in the cells of the liver. The two main types are hepatocellular carcinoma (HCC), which accounts for about 75% of cases, and intrahepatic cholangiocarcinoma. Liver cancer is often linked to chronic liver diseases such as hepatitis B, hepatitis C, and cirrhosis.
Five-Year Survival Rates for Liver Cancer by Stage
| Stage | Survival Rate (%) |
|---|---|
| Localized | 37.3% |
| Regional | 13% |
| Distant | 3.3% |
This chart presents the five-year survival rates for liver cancer based on its stage at diagnosis. Patients diagnosed at the localized stage have the highest survival chances (37.3%), while outcomes drop significantly for regional (13%) and distant (3.3%) stages, underscoring the importance of early detection and treatment.
Survival Rate: What Do the Numbers Say?
First, let’s get something straight: survival rates are statistical averages. They provide general insight but do not predict individual outcomes. Each person’s case is unique — and only the Almighty Allah truly knows the lifespan of every individual.
That said, survival rates are still useful tools in helping patients understand trends and potential outcomes.
According to the American Cancer Society:
| Stage | 5-Year Relative Survival Rate |
|---|---|
| Localized (confined) | About 36% |
| Regional (spread nearby) | Around 13% |
| Distant (spread far) | Close to 3% |
Note: These figures are based on people diagnosed between 2013 and 2019.
Breaking It Down: Survival by Gender and Age
- Men are more commonly diagnosed with liver cancer than women, and generally have slightly lower survival rates.
- Younger patients (under 50) show better survival trends than older individuals due to stronger overall health and better treatment tolerance.
Key Factors That Influence Survival
Several factors affect survival beyond the stage:
- Overall liver function (especially if cirrhosis is present): The liver plays a central role in filtering toxins, producing essential proteins, and metabolizing medications. When cirrhosis (severe liver scarring) is present, it limits the liver’s ability to recover or support aggressive treatments. This often forces physicians to modify or even avoid certain therapies. Patients with well-compensated liver function (e.g., Child-Pugh Class A) typically handle treatment much better than those in advanced liver failure. In real terms, it means that two people with the same tumor size might receive entirely different treatments — simply based on how well their liver is functioning.
- Performance status (how well a person can carry out daily activities): This refers to the patient’s energy levels and independence. A person who walks daily, cooks, and drives can often withstand surgery or chemotherapy better than someone mostly bedbound. The ECOG scale is commonly used to grade this, where 0 means “fully active” and 4 means “completely disabled.” For instance, a patient with ECOG 1 may still work part-time and have a positive prognosis, while a patient with ECOG 3 might need palliative-focused care.
- Response to treatment: Every tumor behaves differently. Some shrink dramatically after therapy, others resist every approach. Imaging tests like MRI and CT scans help evaluate changes, while tumor markers like AFP levels can offer early signals of effectiveness. For example, a patient may see their tumor size cut in half after three rounds of immunotherapy — a good sign. But if there’s no change, doctors may need to switch strategies quickly.
- Type of liver cancer: Not all liver cancers are created equal. While HCC is most common, rare forms like fibrolamellar carcinoma often affect younger adults and may respond better to surgery. In contrast, intrahepatic cholangiocarcinoma typically spreads more aggressively and needs a more complex treatment plan. Knowing the type helps doctors plan the right mix of surgery, chemo, or radiation.
- Genetic markers and tumor biology: The future of cancer care is personal. Tumors are increasingly analyzed for genetic signatures — like PD-L1 expression or mutations in the TERT or TP53 genes — which help guide therapy. For example, a patient whose tumor expresses PD-L1 may benefit greatly from immunotherapy, while another with resistant genes might be directed to clinical trials. It’s a fast-moving field that’s offering more precise and hopeful options every year.
Liver Cancer Survival Rates by Race/Ethnicity in the U.S.
| Race/Ethnicity | Rate (per 100,000) |
|---|---|
| Non-Hispanic White | 10.5 per 100,000 |
| Non-Hispanic Black | 9.5 per 100,000 |
| Hispanic | 6.1 per 100,000 |
| Non-Hispanic Asian or Pacific Islander | 17.5 per 100,000 |
This chart shows liver cancer survival rates in the U.S. by race and ethnicity. Non-Hispanic Asian or Pacific Islander individuals have the highest rate at 17.5 per 100,000, followed by Non-Hispanic Whites and Blacks. Hispanic individuals have the lowest rate, indicating disparities that may reflect access to care, early diagnosis, or socioeconomic factors.
Latest Diagnostic Tools (Accuracy & Cost)
| Diagnostic Method | Description | Accuracy (1–10) | Avg. Cost (USD) |
|---|---|---|---|
| MRI with contrast | Detailed imaging of liver tissues | 9.5 | $1,200–$4,000 |
| CT scan (multi-phase) | Identifies tumors and blood flow | 9.0 | $1,000–$3,500 |
| Liver biopsy | Confirms cancer with tissue sampling | 10.0 | $1,500–$5,000 |
| AFP blood test | Measures alpha-fetoprotein levels (tumor marker) | 7.0 | $30–$150 |
| PET scan | Detects metastasis (spread) | 8.5 | $3,000–$6,000 |
Treatment Innovations Impacting Survival
1. Radioembolization (Y-90 Therapy)
This minimally invasive treatment delivers radioactive Yttrium-90 beads through a catheter directly into the artery feeding the tumor. It’s typically done under light sedation and takes a few hours.
- Effectiveness: Particularly useful for shrinking large or inoperable tumors. Tumor control rates reach up to 80% in localized cases.
- Cost: Ranges from $20,000 to $40,000.
- Complexity: Moderately complex; requires specialized radiology team.
- Availability: Available in major oncology centers.
- Patient Experience: Most patients report minimal pain, though fatigue and nausea can follow for a few days.
2. Immunotherapy (e.g., Nivolumab, Atezolizumab)
This therapy boosts the immune system to recognize and attack cancer cells. Administered via IV infusion every 2–3 weeks.
- Effectiveness: Response rates around 15–20%, with longer control in responders.
- Cost: $10,000–$15,000/month.
- Complexity: Requires regular infusion center visits and monitoring.
- Availability: Widely available in the U.S.
- Patient Experience: Usually well tolerated, though some may develop immune-related side effects like skin rash or fatigue.

3. Targeted Therapy (e.g., Sorafenib, Lenvatinib)
Oral medications that block specific enzymes and blood vessel growth that cancer cells need.
- Effectiveness: Slows progression; improves survival in advanced cases by several months.
- Cost: Around $5,000/month.
- Complexity: Low; oral intake, with regular follow-up.
- Availability: Prescription access in most oncology clinics.
- Patient Experience: Common side effects include diarrhea, hand-foot syndrome, and hypertension.
4. Liver Transplantation
Reserved for patients with early-stage tumors meeting specific criteria (e.g., Milan criteria). Entire liver is replaced with a healthy donor organ.
- Effectiveness: Offers potential cure; 5-year survival rate over 70%.
- Cost: $150,000–$300,000 total.
- Complexity: Highly complex; involves surgery, ICU care, and long-term immunosuppression.
- Availability: Limited by donor organ availability and transplant center access.
- Patient Experience: Recovery involves physical and emotional adjustment, but quality of life often dramatically improves.
5. Microwave Ablation (MWA)
A needle-like probe is inserted into the tumor under imaging guidance, and microwaves heat and destroy cancer cells.
- Effectiveness: Best for small tumors (<3 cm); success rate over 85%.
- Cost: $10,000–$20,000.
- Complexity: Minimally invasive; often outpatient.
- Availability: Increasingly available in urban hospitals.
- Patient Experience: Mild pain at insertion site; quick recovery time.
Liver Cancer Survival Rates by Treatment Type
This chart highlights liver cancer five-year survival rates by treatment type. Radiofrequency ablation offers the highest survival rates for very small tumors (≤2 cm), while surgical resection and liver transplantation show comparable outcomes, making all three viable treatment paths depending on patient and tumor characteristics.
Real Cases from the U.S.
Case 1: Radioembolization Success in Florida
A 62-year-old man from Florida was diagnosed with regional hepatocellular carcinoma (HCC) after experiencing persistent fatigue and unexplained weight loss. His doctors recommended Y-90 radioembolization — a minimally invasive treatment that delivers tiny radioactive beads directly to the tumor. The procedure was performed in a major cancer center and completed without complications. Within three months, his scans showed noticeable shrinkage. Over time, he resumed gardening, traveled with his wife, and even returned to part-time work. With consistent follow-up, he surpassed the five-year survival mark.
Case 2: Transplant and New Life in California
A 45-year-old woman in California discovered her liver cancer during a routine ultrasound related to a family history of cirrhosis. Because the tumor was small and confined, she qualified for a transplant under the Milan criteria. After a short time on the waiting list, she underwent liver transplantation. The procedure and recovery were challenging, but she received strong support from her family and care team. Today, she leads a full, cancer-free life and regularly shares her story to encourage others.
Case 3: Stable Disease Through Immunotherapy in Texas
A 70-year-old veteran in Texas, with a long-standing history of hepatitis C, was diagnosed with advanced liver cancer. Given the extent of disease, surgery was not an option. He started nivolumab infusions every two weeks at a VA oncology center. After 18 months, his tumor stopped growing, a sign of disease stability. The side effects were mild — some fatigue and dry skin — but manageable. Now retired, he mentors other veterans going through cancer treatment.
Editorial Advice
Reyus Mammadli, healthcare advisor, recommends that patients focus less on numbers and more on early detection, overall health, and getting treated in specialized cancer centers. “Statistics offer perspective, not prophecy. Each person’s journey is shaped by timing, genetics, treatment access, and most importantly, divine will.”
Whenever possible, pursue second opinions and explore clinical trials. Remember, medical science is moving fast, and yesterday’s terminal diagnosis could become tomorrow’s success story.
References
- American Cancer Society. “Survival Rates for Liver Cancer.” https://www.cancer.org
- National Cancer Institute. “SEER Cancer Statistics: Liver and Intrahepatic Bile Duct Cancer.” Surveillance, Epidemiology, and End Results Program. https://seer.cancer.gov
- Heimbach, J.K., et al. “AASLD Guidelines for the Treatment of Hepatocellular Carcinoma.” Hepatology, 2018. https://www.aasld.org
- Forner, A., Reig, M., Bruix, J. “Hepatocellular Carcinoma.” Lancet. 2018 Mar 31;391(10127):1301-1314. doi:10.1016/S0140-6736(18)30010-2.
- Llovet, J.M., et al. “Advances in targeted therapies and immunotherapy for hepatocellular carcinoma.” Nat Rev Clin Oncol. 2022 Jan;19(3):151–172. doi:10.1038/s41571-021-00573-3.
- Bruix, J., Sherman, M. “Management of Hepatocellular Carcinoma: An Update.” Hepatology. 2011 Mar;53(3):1020-2. doi:10.1002/hep.24199.
- Mayo Clinic. “Liver cancer – Diagnosis and treatment.” https://www.mayoclinic.org
- U.S. National Library of Medicine. ClinicalTrials.gov. https://clinicaltrials.gov
- Memorial Sloan Kettering Cancer Center. “Liver Cancer Treatment Innovations.” https://www.mskcc.org
- FDA Drug Approvals Database. “Liver Cancer Medications.” https://www.accessdata.fda.gov