Pain around the anus can cause discomfort and affect daily life. It is important to understand the common causes and treatment options available for this condition. Hemorrhoids, anal fissures, anal abscesses and fistulas, anal itching, perianal dermatitis, and proctalgia fugax are some of the common causes of anal pain. Seeking timely medical advice and following proper hygiene practices can help in managing and preventing anal pain. This article will provide insights into these conditions and offer tips for maintaining anal health.
Common causes of anal pain
Common causes of anal pain can include conditions such as hemorrhoids, anal fissures, anal abscesses and fistulas, anal itching, perianal dermatitis, and proctalgia fugax. Hemorrhoids are swollen blood vessels in the rectum or anus. Anal fissures are small tears in the lining of the anus. Anal abscesses and fistulas occur when infections form in the anal glands. Anal itching is often caused by skin irritation. Perianal dermatitis is inflammation of the skin around the anus. Proctalgia fugax is a sudden, intense rectal pain that usually lasts for a short period of time.
Hemorrhoids
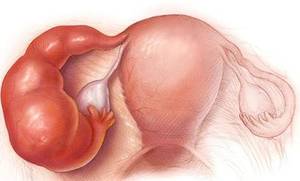
Hemorrhoids are swollen blood vessels in the anus and lower rectum. There are two main types of hemorrhoids: internal and external. Internal hemorrhoids develop inside the rectum and usually go unnoticed unless they become enlarged or prolapsed. External hemorrhoids, on the other hand, occur outside the anus and can be painful or itchy. Treatment options for hemorrhoids include lifestyle changes, over-the-counter creams, and surgical procedures if necessary. It is important to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
Types of hemorrhoids
There are two main types of hemorrhoids: internal and external. Internal hemorrhoids occur inside the rectum, usually causing painless bleeding during bowel movements. They may also protrude outside the anus and become prolapsed. External hemorrhoids, on the other hand, develop under the skin around the anus and can be itchy and painful. It’s important to identify the type of hemorrhoids in order to determine appropriate treatment options. Consulting a healthcare professional is recommended for an accurate diagnosis.
Symptoms and treatment options for hemorrhoids
Symptoms of hemorrhoids often include itching, pain, and discomfort in the anal area. Bleeding during bowel movements may also occur. Treatment options for hemorrhoids include lifestyle changes such as increasing fiber intake and staying hydrated, as well as over-the-counter creams or wipes to alleviate symptoms. In severe cases, medical procedures like rubber band ligation or surgical removal may be necessary. Consult a healthcare professional for a proper diagnosis and personalized treatment plan.
Anal Fissures
Anal fissures are small tears or cuts in the lining of the anus. They are often caused by passing large or hard stools, chronic constipation, or childbirth. Symptoms of anal fissures include pain, bleeding, and itching around the anus. Treatment for anal fissures typically involves lifestyle changes such as increasing fiber intake and using over-the-counter creams or ointments to promote healing. In severe cases, surgical intervention may be necessary. Preventing anal fissures can be achieved by maintaining regular bowel movements and practicing good hygiene in the anal area.
Causes and symptoms of anal fissures
Anal fissures are small tears in the lining of the anus that can cause intense pain. They are often caused by trauma to the anal area, such as straining during bowel movements or passing hard stools. Common symptoms include sharp pain during bowel movements, bleeding, and itching. It is important to keep the area clean to avoid infection. If symptoms persist or worsen, medical attention should be sought.
Treatment and prevention of anal fissures
Treatment for anal fissures typically involves conservative measures and lifestyle modifications. These can include increasing fiber intake through dietary changes or over-the-counter fiber supplements to soften stools and prevent straining during bowel movements. Topical treatments such as numbing creams, ointments, or suppositories may be recommended to alleviate pain and promote healing. Additionally, maintaining good anal hygiene by gently cleaning the area and avoiding excessive wiping can aid in preventing further irritation. In some cases where conservative measures are ineffective, surgical intervention may be required to repair the fissure.
Anal Abscess and Fistula
Anal abscess and fistula are conditions that can cause pain around the anus. An anal abscess is an infected cavity filled with pus, usually caused by a blocked anal gland. On the other hand, an anal fistula is a narrow tunnel that forms between the anal gland and the skin near the anus. Symptoms of both conditions include pain, swelling, and discharge. Treatment options for anal abscesses and fistulas may involve draining the pus and sometimes surgical intervention to prevent recurrence. It is important to seek medical advice for proper diagnosis and appropriate treatment.
Difference between anal abscess and fistula
An anal abscess and a fistula may both involve the anal area, but they are two distinct conditions. An anal abscess is a painful collection of pus that forms near the anus, usually due to an infection. On the other hand, a fistula is an abnormal tunnel that develops between the anal canal and the skin around the anus, according to iytmed.com. While both conditions can cause pain and discomfort, they require different treatment approaches.
Symptoms, diagnosis, and treatment of anal abscess and fistula
Symptoms of an anal abscess may include pain, swelling, redness, and a constant throbbing sensation around the anus. In some cases, fever and chills may also be present. A fistula, which is often the result of an untreated abscess, can cause persistent drainage of pus or stool from an opening near the anus. Diagnosis of these conditions involves a physical examination and sometimes imaging tests. Treatment typically involves surgical drainage of the abscess and in some cases, surgery to repair the fistula.
Anal Itching
Causes and risk factors of anal itching include poor hygiene, excessive moisture, certain skin conditions, and infections. It can also be caused by certain foods or allergies. Home remedies for anal itching include keeping the area clean and dry, using fragrance-free products, avoiding irritating substances, and applying over-the-counter creams or ointments. If the itching persists or worsens, it is advisable to seek medical treatment for a proper diagnosis and further treatment options. Maintaining good anal hygiene and avoiding triggers can help prevent anal itching.
Causes and risk factors of anal itching
The causes of anal itching can vary. One common cause is poor hygiene, as not cleaning the anus properly after bowel movements can lead to irritation. Certain medical conditions, such as hemorrhoids, yeast infections, or sexually transmitted infections, may also cause itching. Skin conditions like eczema or psoriasis can contribute to anal itching as well. Additionally, certain lifestyle factors like excessive sweating or wearing tight clothing can increase the risk of experiencing anal itching. Seeking medical advice is important to determine and address the underlying cause of the itching.
Home remedies and medical treatments for anal itching
There are several home remedies that can help relieve anal itching. These include keeping the anal area clean and dry, using over-the-counter creams or ointments containing hydrocortisone, and avoiding irritating substances such as scented soaps or wipes. In more severe cases, a healthcare professional may prescribe stronger medications like steroid creams or oral antihistamines to reduce itching. It’s important to consult a doctor for a proper diagnosis and treatment plan.
Perianal Dermatitis
Perianal dermatitis is a condition characterized by skin irritation and inflammation around the anus. It can be caused by various factors such as allergies, yeast or bacterial infections, and excessive moisture. Symptoms of perianal dermatitis may include itching, redness, and discomfort. To treat perianal dermatitis, it is important to keep the area clean and dry, avoid irritants, use gentle cleansers, and apply soothing topical creams or ointments. Prevention involves maintaining good hygiene practices and avoiding triggers that may irritate the delicate skin around the anus.
Causes, symptoms, and triggers of perianal dermatitis
Perianal dermatitis is typically caused by excessive moisture, irritation from harsh soaps or wipes, fungal or bacterial infection, or underlying skin conditions such as eczema or psoriasis. Symptoms include redness, itching, burning sensation, and skin irritation in the area around the anus. Triggers for perianal dermatitis can include prolonged sitting, excessive sweating, frequent bowel movements, and certain fabrics or tight clothing that can cause friction and irritation.
Treatment and prevention of perianal dermatitis
Treatment options for perianal dermatitis include topical creams or ointments containing hydrocortisone or zinc oxide to reduce inflammation and soothe the skin. It is important to keep the affected area clean and dry, as moisture can worsen the condition. Avoiding irritants such as scented soaps, bubble baths, and tight-fitting clothing can help prevent flare-ups. Applying a barrier cream before activities that may cause friction, such as exercise, can also be beneficial in preventing perianal dermatitis.
Proctalgia Fugax
Proctalgia Fugax, a condition characterized by sudden and intense rectal pain, is believed to be caused by muscle spasms in the anal area. The exact cause of these spasms remains unknown, but they can be triggered by certain factors such as stress or a history of hemorrhoids. Although the episodes of pain are usually short-lived and resolve on their own, some strategies can help manage and prevent future episodes. These include relaxation techniques, avoiding triggering factors, and maintaining a healthy lifestyle. If the pain becomes persistent or worsens, it is advised to seek medical advice.
Definition and causes of proctalgia fugax
Proctalgia fugax is a condition characterized by sudden, intense pain in the rectum or anus that lasts for just a few seconds to a few minutes. The exact cause of proctalgia fugax is unclear, but it may be due to muscle spasms in the pelvic floor or anal sphincter. Other factors like stress, anxiety, and hormonal changes may also contribute to the onset of proctalgia fugax. Proper diagnosis and management can help alleviate symptoms and prevent future episodes.
Managing and preventing proctalgia fugax episodes
To manage and prevent episodes of proctalgia fugax, individuals can try several approaches. Applying heat to the area using a warm compress or taking a warm bath can help relax the muscles and alleviate pain during an episode. Avoiding triggers like stress, caffeine, and certain medications can help prevent future episodes. If the symptoms persist or worsen, it is important to seek medical advice for proper evaluation and treatment.
Conclusion
When experiencing pain around the anus, it’s important to identify the underlying cause in order to find appropriate treatment. Hemorrhoids, anal fissures, anal abscesses and fistulas, anal itching, perianal dermatitis, and proctalgia fugax are all common causes of anal pain. While some conditions can be managed with home remedies or over-the-counter treatments, others may require medical intervention. It is crucial to seek medical advice if symptoms persist or worsen. Additionally, maintaining good anal hygiene practices and adopting a healthy lifestyle can help prevent and manage anal pain.
When to seek medical advice for anal pain
If you are experiencing anal pain that is severe, persistent, or accompanied by bleeding, it is important to seek medical advice. Additionally, if you notice any changes in your bowel movements, such as sudden diarrhea or constipation, or if the pain is interfering with your daily activities and quality of life, it is recommended to consult a healthcare professional. They can provide an accurate diagnosis and appropriate treatment for your specific condition.
Tips for maintaining anal health and preventing pain
To maintain anal health and prevent pain, it is important to follow these tips:
- Maintain good hygiene: Keep the anal area clean by using gentle, fragrance-free wipes or mild soap and water after bowel movements.
- Use soft toilet paper: Avoid rough or scented toilet paper, as it can irritate the anal area.
- Stay hydrated and eat a high-fiber diet: Drinking plenty of water and consuming fiber-rich foods can help prevent constipation, which can contribute to anal pain.
- Avoid straining during bowel movements: Straining can increase pressure on the anus and contribute to hemorrhoids or fissures. Take your time while on the toilet and consider using a footstool for support.
- Leave out anal sex: it is a God forbidden form of sexual intercourse.
- Stay physically active: Regular exercise helps promote healthy bowel movements and prevents constipation.
- Avoid sitting for long periods: Sitting for extended periods of time can put pressure on the anus. Try to take breaks frequently if you have a job that requires prolonged sitting.
By following these tips, you can maintain good anal health and reduce the risk of experiencing pain or discomfort in the anal area. Remember, if you have persistent or severe anal pain, it is best to seek medical advice for proper diagnosis and treatment.