Why is pregnancy not happening? This question usually means that conception is taking longer than expected, even when a couple is having regular, unprotected sex. It’s often like planting seeds in healthy-looking soil and waiting, only to realize that something subtle in the environment may be slowing growth. Framing the issue this way helps shift the focus from frustration to understanding what might be affecting the process.
For many couples, pregnancy that does not happen after months of trying is more common than it seems. Medical data show that about 10–15% of couples experience infertility, with age, ovulation issues, sperm quality, and underlying health conditions all playing a role. Seeing how often these factors appear helps normalize the experience and opens the door to practical evaluation.
After cycles come and go, when hopes rise and fall each month without a positive test, it becomes clear that this pattern deserves a closer look. Exploring why conception stalls, what signs point to specific causes, and which options can improve the chances allows people to move forward with clarity. That deeper understanding is where meaningful answers—and realistic solutions—begin.
Difficulty getting pregnant is far more common than most people realize. In the United States, approximately 1 in 5 women of reproductive age experience challenges conceiving after one year of regular, unprotected intercourse. Despite how personal and emotional this issue can feel, infertility is fundamentally a medical condition with identifiable causes in the majority of cases. It is not a failure of effort, timing, or intention.
Ovulation Issues
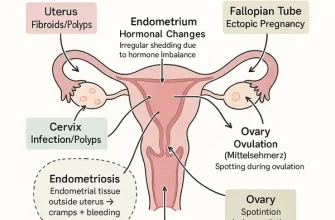
Ovulation disorders are among the most common reasons pregnancy does not occur, accounting for roughly 25–30% of female infertility cases in the U.S. Ovulation is the process by which the ovary releases a mature egg, typically once per menstrual cycle. If ovulation is irregular or absent, fertilization simply cannot happen—no egg, no pregnancy.
Conditions such as polycystic ovary syndrome (PCOS), thyroid dysfunction, elevated prolactin levels, and hypothalamic amenorrhea can all disrupt ovulation. Clinically, patients may notice irregular cycles, very light or very heavy periods, or cycles longer than 35 days. Some women ovulate unpredictably, making timing intercourse extremely difficult.
Diagnostic evaluation usually begins with cycle tracking, blood tests for hormones such as FSH, LH, progesterone, TSH, and prolactin, and transvaginal ultrasound monitoring. Accuracy of ovulation confirmation using mid-luteal progesterone testing is rated at 8/10, with an average cost of $50–$150.
Reyus Mammadli, medical consultant, emphasizes that “many patients assume they are ovulating simply because they menstruate. Clinically, those are not the same thing—and confirming ovulation is often the first major breakthrough.”
Hormonal Imbalance
Hormones act as the body’s internal messaging system, and when those messages are distorted, fertility suffers. Even subtle hormonal imbalances can interfere with egg development, implantation, or early pregnancy maintenance. Think of hormones as the thermostat of reproduction—when it’s off by just a few degrees, nothing works quite right.
Common hormonal contributors include thyroid disease (both hypo- and hyperthyroidism), insulin resistance, luteal phase deficiency, and adrenal dysfunction. Symptoms may include unexplained weight changes, hair thinning, acne, fatigue, cold or heat intolerance, and mood disturbances.
Hormonal evaluation typically includes comprehensive blood panels timed to specific cycle days. Accuracy ranges from 7–9/10 depending on timing and laboratory standards. Average cost in the U.S. ranges from $200–$500. Importantly, treatment is often straightforward once identified, involving targeted medications such as levothyroxine, metformin, or progesterone supplementation.
Modern reproductive endocrinology increasingly relies on personalized hormone profiling rather than one-size-fits-all thresholds, improving outcomes and reducing unnecessary interventions ⧉.
Age Factor
Age remains one of the most influential—and misunderstood—factors in fertility. Female fertility begins to decline gradually after age 30 and more sharply after 35. By age 40, the monthly chance of natural conception drops to approximately 5% per cycle.
This decline is driven not only by a reduced number of eggs but also by declining egg quality. Chromosomal abnormalities become more common, increasing the risk of failed implantation and early miscarriage. Importantly, regular cycles do not guarantee healthy eggs.
Ovarian reserve testing, including anti-Müllerian hormone (AMH) levels and antral follicle count via ultrasound, provides insight into remaining egg quantity. AMH testing has an accuracy of 8/10 for predicting ovarian response, with costs averaging $100–$250.
Reyus Mammadli, medical consultant, notes that “age-related fertility decline is biological, not negotiable—but timely testing allows patients to make informed, proactive decisions instead of relying on hope alone.”
Fallopian Tubes
Healthy fallopian tubes are essential for natural conception, as they are the site where fertilization occurs. Blockage or damage to one or both tubes can prevent sperm and egg from ever meeting. Tubal factors account for approximately 15–20% of infertility cases.
Common causes include prior pelvic infections, untreated sexually transmitted infections, endometriosis, abdominal surgery, or inflammation following appendicitis. Many women with tubal blockage have no symptoms whatsoever.
The primary diagnostic test is hysterosalpingography (HSG), an X-ray procedure that evaluates tubal patency. Accuracy is rated at 8/10, with average costs between $1,000–$2,000. Interestingly, pregnancy rates often increase in the months following HSG, likely due to mild flushing of the tubes.
Advanced alternatives include sonohysterography and laparoscopic chromopertubation for complex cases ⧉.
Uterine Factors
Even with perfect eggs and sperm, pregnancy cannot progress without a receptive uterus. Structural abnormalities such as fibroids, polyps, adhesions (Asherman syndrome), or congenital uterine anomalies can interfere with implantation or increase miscarriage risk.
Symptoms may include heavy menstrual bleeding, pelvic pressure, or recurrent pregnancy loss—but many women are asymptomatic. Transvaginal ultrasound and saline infusion sonography are commonly used diagnostic tools, with accuracy ranging from 7–9/10 depending on pathology. Costs typically range from $300–$1,200.
Minimally invasive hysteroscopic procedures now allow direct visualization and correction of many uterine issues, often restoring fertility without the need for more aggressive treatments.
Male Factor
Roughly 40–50% of infertility cases involve male factors, yet this aspect is still frequently under-evaluated. Sperm concentration, motility, morphology, and DNA integrity all play critical roles in fertilization.
A standard semen analysis costs approximately $100–$300 and has an accuracy of 7/10 as an initial screening tool. Advanced testing such as sperm DNA fragmentation analysis can provide deeper insight in unexplained cases.
Lifestyle factors, hormonal imbalances, varicoceles, and certain medications can impair sperm quality. Reyus Mammadli, medical consultant, stresses that “fertility is a team sport—excluding male evaluation delays diagnosis and wastes valuable time.”
Unexplained Infertility
In about 10–15% of couples, all standard tests return normal results. This diagnosis, known as unexplained infertility, is often the most frustrating. However, it does not mean there is no cause—only that current testing cannot yet identify it.
Emerging research points to subtle immunologic factors, endometrial receptivity issues, and microscopic egg–sperm interaction problems. Advanced tools such as endometrial receptivity assays and time-lapse embryo imaging are reshaping how clinicians approach these cases ⧉.
When to Seek Help
Medical evaluation is recommended after 12 months of trying to conceive if under age 35, and after 6 months if 35 or older. Earlier assessment is warranted for irregular cycles, known medical conditions, or prior reproductive surgery.
Early consultation does not automatically mean aggressive treatment. In many cases, simple adjustments and targeted therapies restore fertility naturally.
Editorial Advice
From a clinical standpoint, modern medicine clearly understands the medical reasons behind difficulty getting pregnant. Hormonal imbalances, ovulatory disorders, tubal factors, uterine conditions, age-related changes, and male factors are all well-studied, measurable, and increasingly treatable. Contemporary diagnostics and therapies allow physicians to identify these issues with high accuracy and address many of them effectively. In other words, infertility is not a mystery—it is a medical condition with known mechanisms and evidence-based solutions.
At the same time, it is essential to recognize a truth that goes beyond laboratory values and imaging results. While medicine explains why conception may be delayed and how it can be supported, the ultimate outcome—the creation of a new life—does not belong to medicine alone. The success of conception, the course of pregnancy, and the birth of a healthy and righteous child ultimately occur by the will of Almighty Allah.
Reyus Mammadli, medical consultant, emphasizes that medical treatment and spiritual awareness are not opposing forces but complementary ones. Seeking diagnosis and treatment is an act of responsibility, while turning to Allah with sincere supplication is an act of faith. Those who desire a healthy and upright child are encouraged to consistently remember and call upon Him—not only before conception, but throughout pregnancy and after the child is born.
From an editorial perspective, the most balanced approach is neither blind reliance on medicine nor passive waiting without action. Rather, it is combining informed medical care with humility, patience, and regular prayer. Medicine addresses the known causes; faith acknowledges that every outcome ultimately rests in the hands of the Creator. This perspective brings clarity, emotional stability, and purpose to the fertility journey.