Back pain that radiates down your leg can be both frustrating and confusing. Is it sciatica? Could it be piriformis syndrome? Though these conditions may feel similar, they are not the same.
Common Symptoms Frequency (%)
| Symptom | Sciatica (%) | Piriformis (%) |
|---|---|---|
| Lower Back Pain | 85% | 20% |
| Leg Pain | 95% | 65% |
| Numbness | 70% | 40% |
| Muscle Weakness | 60% | 20% |
| Buttock Pain | 30% | 90% |
This chart compares the frequency of common symptoms between Sciatica and Piriformis Syndrome. While Sciatica is more associated with leg-related issues and numbness, Piriformis Syndrome shows a much higher correlation with buttock pain. Understanding the distribution of these symptoms helps in differential diagnosis and targeted treatment.
This guide breaks down the differences, diagnosis methods, and treatments to help you understand what’s really behind your pain.
What Is Sciatica?
Sciatica is not a condition in itself but a symptom of an underlying issue. It refers to pain that travels along the path of the sciatic nerve — the longest nerve in the human body, running from your lower back through your hips, buttocks, and down each leg.
Common Causes of Sciatica:
- Herniated disc (most common): When the soft center of a spinal disc pushes out through a tear in its tougher exterior, it can compress the nerve roots leading to sciatica. Symptoms often include sharp pain radiating down one leg, lower back stiffness, tingling, or weakness in the foot or toes.
- Spinal stenosis: A narrowing of the spinal canal that puts pressure on the nerves. People with stenosis usually report pain that worsens when standing or walking, often described as a cramping or burning feeling, which improves when sitting or leaning forward.
- Spondylolisthesis: This occurs when one vertebra slips forward over another, possibly pinching nerve roots. Symptoms can include lower back pain, hamstring tightness, and pain that shoots down one or both legs during physical activity.
- Degenerative disc disease: As discs naturally wear down with age, they may lose height and elasticity, which can irritate nearby nerves. Symptoms are often chronic and include intermittent sciatica, dull or aching lower back pain, and worsened pain after sitting.
- Tumors (rare): Though uncommon, tumors in the spine can compress the sciatic nerve. Symptoms may be more persistent and progressive, including constant back pain not relieved by rest, night pain, and possible neurological signs like muscle weakness or loss of bladder/bowel control.
Typical symptoms: Sharp, shooting pain, numbness, tingling, or muscle weakness along the sciatic nerve pathway.
Most Common Causes (%)
| Cause | Sciatica (%) | Piriformis (%) |
|---|---|---|
| Herniated Disc | 70% | 10% |
| Muscle Tightness | 15% | 60% |
| Trauma | 10% | 15% |
| Overuse Injury | 5% | 15% |
This chart presents the most common causes of Sciatica and Piriformis Syndrome. Herniated discs are the leading cause of Sciatica, while muscle tightness dominates as the primary cause of Piriformis Syndrome. Trauma and overuse injuries contribute modestly to both conditions.
What Is Piriformis Syndrome?
Piriformis syndrome happens when the piriformis muscle, located deep in the buttock, spasms or becomes tight and compresses the sciatic nerve.
What Triggers It?
- Muscle trauma or overuse — This can result from a sudden impact or repetitive strain, such as falling directly on the buttock or overworking the hip rotators during exercise. The piriformis muscle may swell or tighten in response, leading to sciatic nerve compression. People often report a sudden, localized ache followed by radiating pain down the leg.
- Prolonged sitting — Especially on hard surfaces or with poor lumbar support, this compresses the gluteal region and piriformis muscle for extended periods. Common in drivers, office workers, and long-haul travelers. Symptoms include numbness in the buttocks, a “pins and needles” sensation, and increasing discomfort that improves with walking or standing.
- Poor posture — Slouching, pelvic misalignment, and uneven weight distribution can strain the piriformis muscle. Over time, this leads to muscle fatigue and reactive tightening. Associated symptoms may include chronic lower back tension, asymmetric hip alignment, and discomfort when crossing legs.
- Athletic strain — Activities involving repetitive leg motion (e.g., running, cycling, rowing) can overload the piriformis, especially if stretching is skipped. The result is deep gluteal pain, often mistaken for hamstring or sacroiliac joint issues. Some athletes notice difficulty sprinting or kicking due to tightness and tingling along the posterior thigh.
Typical symptoms: A dull ache in the buttocks, pain radiating down the back of the thigh, and difficulty sitting for extended periods.
How Can You Tell Them Apart?
Here’s a handy comparison table to highlight the key differences:
| Feature | Sciatica | Piriformis Syndrome |
|---|---|---|
| Origin of Compression | Spinal nerve root | Piriformis muscle |
| Pain Location | Lower back, buttock, leg | Buttock, sometimes thigh |
| Triggering Activity | Lifting, bending, herniated disc | Sitting, climbing stairs |
| Physical Exam Sign | Positive straight leg raise | Tender piriformis muscle |
| Imaging | MRI/CT often reveals cause | Often normal imaging |
Diagnostic Methods
1. Physical Exam
A doctor will test muscle strength, reflexes, and nerve sensitivity.
- Accuracy: 6/10
- Cost: Included in most primary visits
2. MRI (Magnetic Resonance Imaging)
Useful for visualizing herniated discs or spinal issues.
- Accuracy: 9/10
- Cost: $1,000 – $5,000 (USD) / €920 – €4,600 (EUR)
3. CT Scan
Helpful when MRI is not an option.
- Accuracy: 8/10
- Cost: $500 – $3,000 (USD) / €460 – €2,750 (EUR)
4. Electromyography (EMG)
Measures electrical activity of muscles and nerves.
- Accuracy: 7/10
- Cost: $200 – $1,200 (USD) / €185 – €1,100 (EUR)
5. Piriformis Injection Test
A steroid is injected into the piriformis muscle. If pain decreases, the diagnosis is likely piriformis syndrome.
- Accuracy: 8/10
- Cost: $400 – $800 (USD) / €370 – €730 (EUR)
Treatment Options
Treatment Preference Among Patients (%)
| Treatment | Sciatica (%) | Piriformis (%) |
|---|---|---|
| Physical Therapy | 60% | 75% |
| Pain Medication | 55% | 40% |
| Surgery | 20% | 5% |
| Injections | 30% | 25% |
This chart compares treatment preferences among patients with Sciatica and Piriformis Syndrome. Physical therapy is the top choice for both conditions, though more prominent in Piriformis cases. Surgery is significantly less favored, especially for Piriformis, suggesting a preference for conservative management strategies.
Sciatica Treatment
Medications for Sciatica
Common medications for sciatica include nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, muscle relaxants such as cyclobenzaprine, and nerve pain modulators like gabapentin.
- Procedure: Typically prescribed for daily use, over 1–3 weeks. Gabapentin may be used long-term under supervision.
- Effectiveness: Moderate (6.5/10), often effective at managing symptoms but not addressing root cause.
- Cost: $20–100 (USD) / €18–90 (EUR) monthly, depending on the drug and dosage.
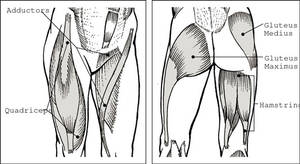
Physical Therapy for Sciatica
Therapy focuses on correcting posture, improving spinal alignment, and strengthening the core to relieve nerve pressure. McKenzie exercises are particularly helpful for disc-related issues.
- Key Techniques: Core engagement, pelvic tilts, back extensions, McKenzie method for disc decompression.
- Effectiveness: High (8/10), especially when done consistently for 6–12 weeks.
- Cost: $75–150 (USD) / €70–130 (EUR) per session. Most patients attend 2–3 sessions per week initially.
Spinal Decompression Therapy
This non-surgical treatment gently stretches the spine using a motorized traction table to relieve pressure on spinal discs.
- Procedure: 20–30 minute sessions, typically over 4–6 weeks.
- Effectiveness: High (8.5/10) for herniated or bulging discs causing sciatica.
- Cost: $100–250 (USD) / €90–230 (EUR) per session. Often sold in treatment packages.
Epidural Steroid Injections
Injections such as Depo-Medrol are used to reduce inflammation around the irritated sciatic nerve.
- Procedure: Outpatient; guided by fluoroscopy or CT for accuracy.
- Effectiveness: Very high (9/10) in acute flare-ups; effects may last weeks to months.
- Cost: $500–1,500 (USD) / €460–1,400 (EUR) per injection.
Surgical Options for Severe Sciatica
In cases where conservative treatment fails, surgical procedures like microdiscectomy (removing part of a herniated disc) or laminectomy (removing part of the vertebra to ease pressure) are considered.
- Procedure: Involves general anesthesia and hospital stay; full recovery can take weeks to months.
- Effectiveness: High (8.5–9/10), especially when nerve root compression is clearly visible on imaging.
- Cost: $15,000–50,000 (USD) / €13,800–46,000 (EUR), including hospital and surgeon fees.
Piriformis Syndrome Treatment
Medications for Piriformis Syndrome
First-line treatment often includes nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen, and muscle relaxants like cyclobenzaprine. These help reduce muscle spasms and inflammation.
- Effectiveness: Moderate (6/10) — best for short-term relief.
- Procedure: Oral medications, typically 7–14 days per cycle.
- Cost: $10–$50 (USD) / €9–45 (EUR) for a 2-week supply.
Physical Therapy
Physical therapy focuses on stretching and relaxing the piriformis muscle, improving posture, and strengthening surrounding muscles to reduce nerve pressure.
- Key Techniques: Guided piriformis stretches, trigger point therapy, posture correction, deep tissue massage.
- Effectiveness: High (8/10) when consistently followed over 4–8 weeks.
- Cost: $75–150 (USD) / €70–130 (EUR) per session; often 8–12 sessions recommended.
Ultrasound-Guided Injections
A corticosteroid or anesthetic is injected directly into the piriformis muscle under ultrasound guidance to reduce inflammation and pain.
- Procedure: Outpatient, local anesthesia, real-time imaging.
- Effectiveness: Very high (9/10) when pain is due to inflammation.
- Cost: $400–800 (USD) / €370–730 (EUR) per treatment.
Shockwave Therapy
High-energy acoustic waves are directed at the piriformis region to promote healing and release tight muscle tissue.
- Procedure: Non-invasive, 3–6 sessions recommended.
- Effectiveness: Moderate to high (7.5/10), especially for chronic cases.
- Cost: $100–250 (USD) / €90–225 (EUR) per session.
Piriformis Release Surgery
This is a rare but effective solution when all non-surgical methods fail. The piriformis muscle is partially released to stop it from compressing the sciatic nerve.
- Procedure: Performed under general anesthesia; requires physical rehab post-op.
- Effectiveness: High (8.5/10) in carefully selected patients.
- Cost: $7,000–20,000 (USD) / €6,400–18,500 (EUR) total, including hospital fees.
Case Examples
- Male, 52, Dallas, TX: Diagnosed with sciatica caused by L5-S1 disc herniation. Underwent physical therapy and epidural injections. Pain decreased by 70%.
- Female, 38, Portland, OR: Persistent buttock pain while sitting. MRI normal. Piriformis injection reduced pain significantly. Diagnosed with piriformis syndrome.
Prevention Tips
- Here are practical, everyday steps to prevent both sciatica and piriformis syndrome:
- Stretch daily: Focus on hamstrings, hip flexors, and piriformis. Even 10 minutes in the morning and evening can help. Try seated or lying piriformis stretches if standing is difficult.
- Take breaks if you sit a lot: Every 30–60 minutes, stand up, walk around, or do a few gentle squats or hip rolls. Set a phone timer to remind you.
- Upgrade your chair: Use an ergonomic chair with lumbar support, or place a small rolled towel behind your lower back. Adjust seat height so knees are level with hips.
- Strengthen key muscles: Do simple core and glute exercises like bridges, bird-dogs, and planks 3–4 times per week. These muscles stabilize your spine and pelvis.
- Be mindful of movement: Avoid repeatedly twisting at the waist or lifting with a rounded back. Use proper form when exercising, and don’t ignore small aches — they can turn into big ones.
Editorial Advice
Sciatic pain can be a real pain in the… back — and leg. Knowing the difference between sciatica and piriformis syndrome can save you time, money, and unnecessary discomfort.
Reyus Mammadli, healthcare advisor, recommends: “Start with a comprehensive evaluation. Don’t ignore persistent pain. It may not be your back at all — sometimes, it’s that small piriformis muscle causing all the drama.”
If you’re experiencing radiating leg pain, seek care from a neurologist or orthopedist. Remember, pain relief starts with pinpointing the true cause.
References
- Harvard Health Publishing. “Piriformis syndrome.” https://www.health.harvard.edu/pain/piriformis-syndrome
- Cleveland Clinic. “Sciatica.” https://my.clevelandclinic.org/health/diseases/12792-sciatica
- American Academy of Orthopaedic Surgeons (AAOS). “Herniated Disc.” https://orthoinfo.aaos.org/en/diseases–conditions/herniated-disc
- Spine-health. “Piriformis Syndrome vs. Sciatica.” https://www.spine-health.com/conditions/sciatica/piriformis-syndrome-vs-sciatica
- National Institute of Neurological Disorders and Stroke (NINDS). “Low Back Pain Fact Sheet.” https://www.ninds.nih.gov/low-back-pain-fact-sheet
- PubMed Central (PMC). “Effectiveness of physical therapy in the treatment of piriformis syndrome: a systematic review.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7082421
- Radiopaedia. “Sciatica.” https://radiopaedia.org/articles/sciatica
- Mayo Clinic. “Spinal stenosis.” https://www.mayoclinic.org/diseases-conditions/spinal-stenosis
- Medscape. “Piriformis Syndrome Clinical Presentation.” https://emedicine.medscape.com/article/1242983-clinical