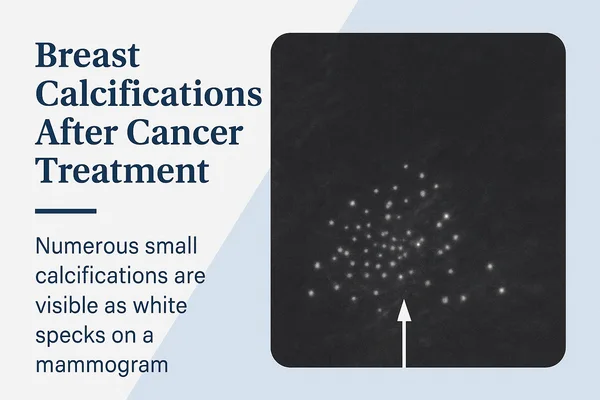
You’ve just read the word “calcifications” on your post-cancer mammogram report — and now your mind is doing backflips. Sound familiar? You’re not alone. These tiny calcium spots in the breast often sound scarier than they are, but understanding them is your first step in staying ahead.
Time to Development of Benign vs. Malignant Calcifications Post-Treatment
This chart compares the median time in months to the development of benign and malignant calcifications following treatment. Malignant calcifications tend to appear later than benign ones, indicating a longer post-treatment latency period.
So, what exactly are breast calcifications? Picture microscopic flecks of calcium that show up as white dots on a mammogram. They’re incredibly common, especially in women over 50, and most of the time they’re harmless. But — and here’s the catch — when they appear after breast cancer treatment, they can raise some red flags. That’s because certain patterns, shapes, or clusters of these deposits may point to something more serious, like a local recurrence or pre-cancerous change.
The good news? Advances in imaging and diagnostic tools mean doctors can now read these patterns with impressive precision. Spotting suspicious microcalcifications early gives you a long-term edge in managing your breast health. And no — you don’t need to panic, but you do need to be informed.
Let’s break it all down together, one step at a time.
These microcalcifications can be benign (harmless), suspicious, or sometimes even signal recurrence. The shape, size, and pattern on a mammogram are what radiologists pay close attention to. Think of it like forensic analysis in CSI, but for your breasts.
How Common Are Calcifications After Breast Cancer?
Turns out, pretty common. Studies show that up to 30% of women develop new calcifications after breast-conserving therapy (BCT), like lumpectomy and radiation. [Source: American Journal of Roentgenology]
Most of these cases are benign. But the key is differentiation — which brings us to imaging.
Resolution of Benign Calcifications Post-Neoadjuvant Chemotherapy
The chart illustrates the degree of resolution of benign calcifications after neoadjuvant chemotherapy. While the majority showed partial resolution, a significant portion had no change, and only a small minority experienced complete resolution.
Diagnosing Post-Cancer Calcifications: Not All Are Created Equal
When calcifications are spotted during routine follow-up mammograms, radiologists use high-resolution imaging and classification systems like BI-RADS to categorize findings.
Imaging Methods:
| Method | Description | Accuracy (1-10) | Average Cost (USD) |
|---|---|---|---|
| Digital Mammography | Standard tool for follow-ups | 7 | $150–$300 |
| 3D Mammography (Tomosynthesis) | Better for dense breasts | 8 | $250–$500 |
| Breast MRI | Great for soft tissue contrast | 9 | $1,000–$2,500 |
| Stereotactic Biopsy | When something looks fishy | 10 | $1,500–$2,200 |
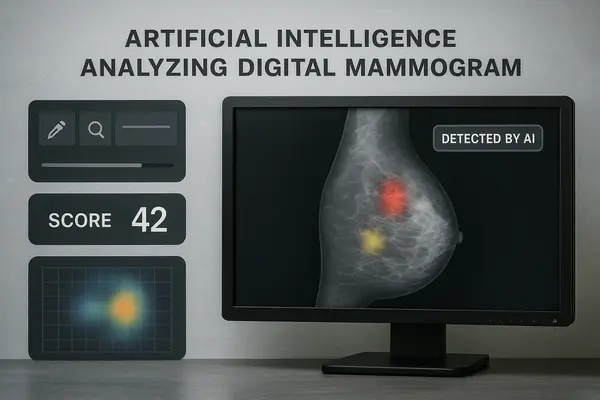
Modern AI tools like iCAD and Transpara can also help radiologists detect and interpret calcifications faster and more accurately.
What Do Suspicious Calcifications Look Like?
Radiologists look for clues:
- Tight clusters
When calcifications appear in tight groups, especially within a small area, they could indicate abnormal cell activity. You won’t feel this with your hand, but your radiologist can spot it easily on a mammogram. There may not be external symptoms, but in some rare cases, subtle skin dimpling or a firmer area under the skin might occur. - Irregular shapes
Normal calcifications tend to be round or oval. When the shapes become jagged, angular, or oddly shaped, it can raise concern. These can’t be seen or felt by touch but are flagged during imaging. If you’ve noticed asymmetry in your breast appearance or a newly thickened area, bring it up. - Linear or branching patterns
These are the most concerning, as they can suggest calcifications forming inside ducts — a potential sign of ductal carcinoma in situ (DCIS). You won’t feel pain or see color changes with this, but a mammogram may reveal it. Occasionally, this may be accompanied by nipple discharge (particularly if bloody or clear) or skin retraction.
If your report mentions any of these findings, it doesn’t mean you have cancer — it simply means more information is needed. Your doctor may suggest a follow-up mammogram, a 3D scan, or a biopsy just to make sure.
Real Cases from the U.S.
- Female, 64, Phoenix, AZ: New calcifications appeared 18 months after lumpectomy. Biopsy confirmed benign fibrocystic changes.
- Female, 51, Chicago, IL: Detected linear calcifications 2 years post-radiation. Diagnosed as ductal carcinoma in situ (DCIS) recurrence.
- Female, 57, Atlanta, GA: Clustered calcifications seen on 3D mammogram. Underwent vacuum-assisted biopsy — results were benign.
Treatment Options: When Is Action Required?
If calcifications are benign, no treatment is needed — just regular monitoring. But if they’re suspicious or cancerous, here’s what might come next:
Surgical Biopsy or Excision
This involves removing the suspicious area of breast tissue through a small operation, often done under local anesthesia. It usually takes under an hour and is performed in an outpatient setting.
- What it includes: Image-guided localization (e.g., with wire or magnetic seed), small incision, tissue removal
- Effectiveness: High diagnostic accuracy; can rule out or confirm cancer
- Cost in the U.S.: $2,000–$5,000
- Recovery & side effects: Soreness, mild bruising, risk of infection (rare); recovery in a few days
- Repeat procedures? Only if margins are unclear or new calcifications develop
Targeted Radiation Therapy
Used if the calcifications indicate a local recurrence. This type of radiation is focused specifically on the area of concern, sparing the rest of the breast.
- What it includes: CT planning scan, 5–10 short daily sessions (vs. traditional 20–30)
- Effectiveness: Proven to reduce risk of local recurrence
- Cost in the U.S.: $6,000–$12,000 total (depending on protocol)
- Side effects: Fatigue, skin irritation, breast firmness
- Repeat procedures? Rare, but possible if recurrence happens in a different area
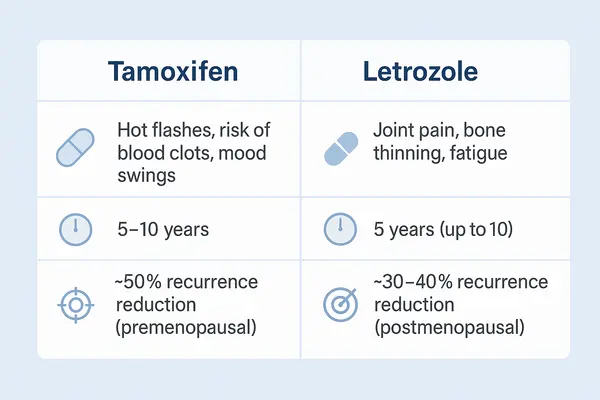
Endocrine (Hormone) Therapy
Recommended when the calcifications are linked to hormone-receptor-positive breast cancer. Medications are taken daily for 5–10 years to reduce recurrence risk.
- What it includes: Oral drugs like tamoxifen or aromatase inhibitors (letrozole, anastrozole)
- Effectiveness: Can reduce recurrence by up to 50% in hormone-positive patients
- Cost in the U.S.: $100–$500/month depending on insurance and brand
- Side effects: Hot flashes, joint pain, mood changes, bone thinning
- Repeat or change? Sometimes meds are changed due to side effects or new data
It’s completely normal to feel overwhelmed, but knowing the roadmap ahead — and the reasoning behind each option — helps you feel more in control.
Can Technology Help Reduce the Risk of Missed Diagnoses?
Absolutely. New technologies don’t just “predict risk” — they help reduce the chances of missing a problem early and guide doctors in making faster, more accurate decisions.
These tools are based on artificial intelligence (AI), which works a bit like a highly trained assistant with a photographic memory. It reviews thousands of past mammograms and learns to spot the tiniest patterns linked with recurrence or new changes — even ones that might be easy to miss by the human eye.
Tools Making a Difference:
- Koios DS: An FDA-cleared AI system that assists doctors during breast ultrasound evaluations. It highlights areas that may need closer examination — think of it like Google Maps alerting you to a traffic jam before you see it.
- Transpara: Supports mammogram readings by assigning a risk score to areas of concern. It ranks findings so radiologists can prioritize what to examine more closely.
- iCAD: Uses deep-learning algorithms to scan mammograms for suspicious patterns, helping to improve early detection and reduce false negatives.
These systems don’t replace your radiologist — they act as a second pair of eyes. And when it comes to your health, having backup like that can make a real difference.
Prevention and Monitoring: What Can You Do?
You can’t always prevent breast calcifications, but you can absolutely take smart steps to monitor them and catch any problems early.
1. Stick to Your Imaging Schedule
After breast cancer treatment, follow-up imaging is usually recommended every 6 to 12 months for the first 5 years. These regular mammograms — sometimes paired with breast ultrasounds or MRIs — are your early-warning system. Be sure to:
- Confirm appointments well in advance
- Ask if you’re due for 3D mammography or MRI based on your breast density
- Bring previous imaging results with you, especially if you’re switching clinics
2. Understand BI-RADS Scores
BI-RADS stands for Breast Imaging Reporting and Data System. It’s a scoring system used by radiologists to describe the level of concern seen on your mammogram:
- BI-RADS 1: Negative (everything looks fine)
- BI-RADS 2: Benign (not cancer)
- BI-RADS 3: Probably benign (needs short-term follow-up)
- BI-RADS 4 or 5: Suspicious or highly suggestive of cancer (biopsy needed)
Ask your doctor which BI-RADS score you received and what it means for your personal risk level. It’s okay to write down the explanation or ask for a printed summary.
3. Report Any Changes Immediately
You’re the first to know if something feels different. Tell your healthcare provider if you notice:
- New lumps
- Skin changes (like dimpling or redness)
- Nipple discharge
- Persistent pain in one spot
Even if you’ve just had a mammogram, new symptoms deserve a re-check.
4. Keep a Personal Health Journal
Document your imaging results, doctor visits, and any symptoms you notice. This helps:
- Spot trends over time
- Communicate more clearly with your medical team
- Prepare for second opinions if needed
You don’t need a fancy app — even a simple notebook works.
5. Ask Questions — It’s Your Right
If you’re unsure why a certain scan was ordered or what “calcification cluster” means, ask. There are no dumb questions when it comes to your health. Try questions like:
- “What kind of calcifications are these?”
- “Do I need a biopsy, or just more frequent follow-up?”
- “Are these new or stable compared to last year?”
Being proactive doesn’t mean being paranoid — it means being informed.
Editorial Advice
Reyus Mammadli, medical consultant, recommends: “Never assume all calcifications after breast cancer are harmless. But don’t lose sleep over them either. Imaging technology today is more precise than ever, and early action saves lives.”
Other tips from our editorial team:
- Don’t skip annual mammograms, even if you feel fine
- Track your BI-RADS scores over time — knowledge is power
- Get a second opinion if results are unclear or if something doesn’t sit right with you
Breast calcifications can seem mysterious or even scary, especially after a cancer diagnosis. But with sharp imaging, smart tech, and informed decisions, you’re in the driver’s seat — not the passenger.
Malignancy Rates of New Calcifications by Location Relative to Lumpectomy Site
| Location | Malignancy Rate (%) |
|---|---|
| Within Lumpectomy Site | 1.5% |
| Outside Lumpectomy Site | 37.5% |
This chart compares the malignancy rates of new calcifications based on whether they appeared within or outside the lumpectomy site. New calcifications outside the lumpectomy site show a significantly elevated malignancy risk, visually emphasized by extended bar lengths.
References and Sources
- American College of Radiology (ACR). BI-RADS Atlas — Breast Imaging Reporting and Data System. Available at: https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Bi-Rads
- American Journal of Roentgenology. “New Calcifications After Breast-Conserving Therapy: Outcomes and Follow-Up.” AJR Am J Roentgenol. 2018;210(4):929–938. DOI: https://doi.org/10.2214/AJR.17.19015
- Mayo Clinic. “Breast calcifications: What causes them?” Reviewed by Dr. Sandhya Pruthi. Available at: https://www.mayoclinic.org/diseases-conditions/breast-cancer/expert-answers/breast-calcifications/faq-20058484
- Koios Medical. FDA Clearance for Koios DS Breast. Available at: https://www.koiosmedical.com
- iCAD Inc. “Artificial Intelligence for Breast Imaging.” Product overview and clinical validation. Available at: https://www.icadmed.com/breast-health-solutions.html
- Transpara by ScreenPoint Medical. “AI-powered decision support for breast cancer detection.” Available at: https://screenpoint-medical.com
- National Cancer Institute (NCI). Breast Cancer Treatment PDQ®. Available at: https://www.cancer.gov/types/breast/patient/breast-treatment-pdq
- National Comprehensive Cancer Network (NCCN). NCCN Guidelines for Patients®: Breast Cancer. Available at: https://www.nccn.org/patients/guidelines/content/PDF/breast-patient.pdf
- Radiological Society of North America (RSNA). “Understanding Your Mammogram Report.” Available at: https://www.radiologyinfo.org/en/info/mammo
- Centers for Medicare & Medicaid Services (CMS). Healthcare Costs for Imaging Services. Available at: https://www.cms.gov