Warfarin-induced skin necrosis (WISN) is an uncommon and severe side effect that can occur in patients who are being treated with warfarin, a medication that thins the blood and is often prescribed to prevent blood clots in conditions like atrial fibrillation, deep vein thrombosis, and pulmonary embolism.
Pathophysiology of Warfarin-Induced Necrosis
Warfarin-induced necrosis occurs due to an imbalance in the body’s clotting and anticoagulation processes. Warfarin functions by blocking vitamin K-dependent clotting factors, such as Factors II, VII, IX, and X, which play a critical role in blood clotting.
In the beginning of warfarin treatment, there is a temporary increase in blood clotting known as hypercoagulability. This is because the natural inhibitors of clotting factors, including Protein C and Protein S, have shorter half-lives than the clotting factors themselves. This results in a quicker depletion of these inhibitors when warfarin therapy is started, leading to a temporary imbalance in blood clotting.
Risk Factors Associated with WISN
- High Loading Dose: Starting warfarin therapy with a high loading dose can precipitate WISN.
- Protein C Deficiency: Patients with a deficiency in Protein C or Protein S are more susceptible to WISN.
- Interruption of Vitamin K Administration: Abrupt cessation of dietary vitamin K or discontinuation of vitamin K administration can lead to a more severe imbalance and increase the risk of necrosis.
- Concomitant Risk Factors: The presence of other risk factors such as obesity, advanced age, or a history of previous thromboembolism may elevate the risk for WISN.
Clinical Presentation
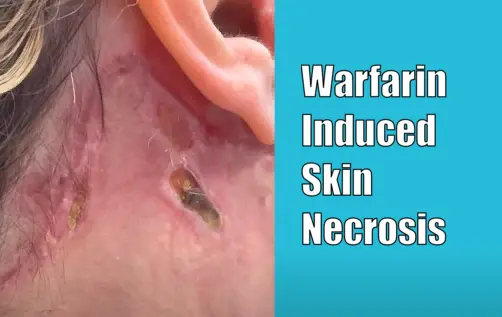
- Localized Pain: Patients typically experience severe pain at the affected site, often within 3 to 10 days after initiating warfarin therapy.
- Skin Changes: Initial reddish petechiae can progress to a hemorrhagic bullae and then to full-thickness skin necrosis.
- Common Areas Affected: Warfarin-induced necrosis commonly affects areas with high fat content, such as the breasts, thighs, or buttocks.
Management and Treatment
- Discontinuation of Warfarin: Immediate cessation of warfarin is imperative once WISN is diagnosed.
- Vitamin K Administration: Administration of vitamin K helps to counter the effects of warfarin and restore the levels of clotting factors.
- Heparin: The initiation of alternative anticoagulation with heparin may be necessary, as it does not affect Protein C and Protein S levels.
- Wound Care: Proper care for necrotic tissue is required, and in severe cases, surgical debridement may be necessary.
Prevention
Preventive strategies for warfarin-induced necrosis include:
- Gradual initiation of warfarin therapy with low initial doses
- Early use of heparin when starting warfarin
- Monitoring Protein C and Protein S levels in high-risk patients
- Patient education about signs and symptoms of WISN
Conclusion
WISN, though uncommon, is a severe side effect of warfarin therapy requiring prompt recognition and treatment. Adequate prevention strategies and patient education are essential components in the management of patients on warfarin to mitigate the risks of this potential complication.