Kidney infection (pyelonephritis) is a type of urinary tract infection (UTI) that typically starts in your urethra or bladder and journeys to one or both of your kidneys.
A kidney infection needs timely medical attention. If not treat it effectively, a kidney infection can completely harm your kidneys or the bacteria can spread to your blood stream and trigger a lethal infection.
Kidney infection treatment, which typically includes antibiotics, might need hospitalization.
The most of urinary tract infections (UTIs) involve just the bladder and urethra (the lower urinary system). Pyelonephritis (kidney infection) results when a UTI progresses to involve the upper urinary system (the kidneys and ureters).
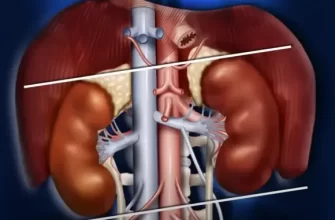
The kidneys filter the blood to produce urine. Two tubes called the ureters carry urine from the kidneys to the bladder. Urine takes a trip from the bladder from the body through the urethra.
The main of cases of kidney infection are problems of typical bladder infections. Bacteria get in the body from the skin around the urethra. They then take a trip up the urethra to the bladder.
Often, bacteria leave the bladder and urethra, traveling up the ureters to one or both kidneys.
Pyelonephritis is a potentially major kidney infection that can infect the blood, causing severe illness. Fortunately, pyelonephritis is usually curable with antibiotics.
The urethra is much shorter in women than in men, which is one reason why women are more susceptible to UTIs and pyelonephritis.
Symptoms of Kidney Infection
At least half of women have experienced the pain with urination caused by a urinary tract infection: painful, urgent, or regular urination.
Kidney infection may begin with comparable symptoms. Nevertheless, once the infection has actually infected the kidney, signs of more severe health problem typically result. They include:
- Back pain or flank pain
- Fever (typically present) or chills
- Feeling sick (malaise).
- Nausea and vomiting.
- Confusion (particularly in the senior).
Kidney infection may cause visible modifications in the urine, such as:
- Blood in the urine (hematuria).
- Cloudy or foul-smelling urine.
- Pain when urinating.
- Increased frequency or urgency of urination.
Causes of Kidney Infection
Most often, the bacteria that cause kidney infection are the same as those that cause regular urinary tract infections. Bacteria discovered in stool (such as E. coli or klebsiella) are most common. Uncommonly, bacteria from the skin or the environment cause pyelonephritis.
Conditions that produce minimized urine circulation make kidney infection most likely. When urine flow slows or stops, bacteria can more quickly take a trip up the ureters. Some causes of urine obstruction include:
- Benign prostatic hypertrophy (BPH).
- Abdominal or pelvic masses (as from cancer).
- Stones in the bladder, ureters, or kidneys.
Kidney stones add to pyelonephritis by containing a location for bacteria to grow while evading the body’s defenses.
Individuals with diabetes or conditions that impair the body immune system are more likely to obtain pyelonephritis.
How Pyelonephritis Is Diagnosed
Doctors may rely on different tests to detect pyelonephritis:
History. Informing the story of your disease and specific symptoms helps a doctor make the medical diagnosis of pyelonephritis.
Physical exam. A doctor keeps in mind an individual’s basic appearance, crucial signs, and presses over the kidneys to look for tenderness.
Urinalysis. In pyelonephritis, tiny analysis of the urine practically always reveals signs of infection. This can include an excess of leukocyte and bacteria.
Urine culture. Within days, bacteria in urine might grow on a culture meal, enabling the best antibiotic to be chosen.
Blood cultures. If pyelonephritis has actually infected the blood, blood cultures can find this and guide treatment.
Computer tomography (CT scan). A scanner takes a rapid series of X-rays, and a computer system creates in-depth pictures of the abdominal area and kidneys. A CT scan is not essential to identify pyelonephritis, but in some cases helps.
Kidney ultrasound. A probe directs high-frequency sound waves through the skin, creating pictures of the kidneys and ureters. Ultrasound can assist recognize abscesses, stones, and blockages.
In addition to identifying kidney infection itself, doctors look for any conditions that make pyelonephritis most likely. For example, kidney stones or abnormality of the urinary tract can increase the opportunity of an infection. Both are potentially correctable, which will minimize the possibilities of future kidney infections.
Treatment of Kidney Infection
Pyelonephritis (kidney infection) is a severe infection that always requires treatment with antibiotics. Home solutions alone aren’t effective or recommended for kidney infection.
For a lot of cases of kidney infection, hospitalization isn’t really needed. Home treatment is suitable if a person is able to navigate and can consistently take oral antibiotics. For example, they must not be confined to bed or regularly vomiting.
Hospitalization is needed to deal with more severe kidney infection, however. Providing antibiotics intravenously in the health center makes sure that the medicine is reaching the kidneys.
Antibiotics are usually recommended for an overall of at least seven days. Part of this course of treatment may be given up the hospital intravenously; the remainder of the treatment might be taken in your home through pills.
In unusual cases, pyelonephritis may progress to form a pocket of infection (abscess). Abscesses are tough or impossible to treat with antibiotics alone and must be drained. Most often, this is done with a tube inserted through the skin on the back into the kidney abscess (a procedure called a nephrostomy).
Acute and Chronic Pyelonephritis
Many cases of pyelonephritis are acute, implying abrupt and self-limited. After cure with antibiotics, there is hardly ever any enduring damage to the kidneys. Most individuals do not develop pyelonephritis again.
Chronic (lasting) pyelonephritis is an uncommon condition, usually brought on by abnormality in the kidney. Repetitive UTIs (normally in children) lead to progressive damage and scarring in the kidney. This can ultimately cause kidney failure. Normally, chronic pyelonephritis is found in youth.









Hi my name is Danisha babitsch. I’ve been having really bad pain in my back my my ribs I have a broken rib I gotten beat up from my auntie a year ago but my ribs hasn’t heal right I was on Antibiotics 3 times for my kidneys I was taken to the hospital by Ambulance on Valentine’s Day when I fell I couldn’t pull myself up from the floor it’s was to much pain I tried screaming for help I couldn’t speak I was crying and couldn’t breath so I hit the floor and the glass door so loud then finally on the top of my lungs and screm it’s was 7:30 in the morning on valentine day I’ve been getting sick a lot I’ve been falling asleep when I’m not tired or when I’m doing something I would pass out I’ve been bleeding for 3 days now. And my spine hurts. I’ve had a headache for the last week I can’t think or eat well. I have asthma my broken rib is under my left rib I have hard time breathing I don’t know what’s going on with me. I see my family doctor tomorrow. I’m 21 years old please get back to me. I’m scared. And worried I don’t know what to do